More than half of people who receive antibiotics to treat appendicitis do not see their disease come back 10 years after the initial illness, a new study shows. The data come from one of the first clinical trials of the approach and bolster newly updated guidelines for treating appendicitis.
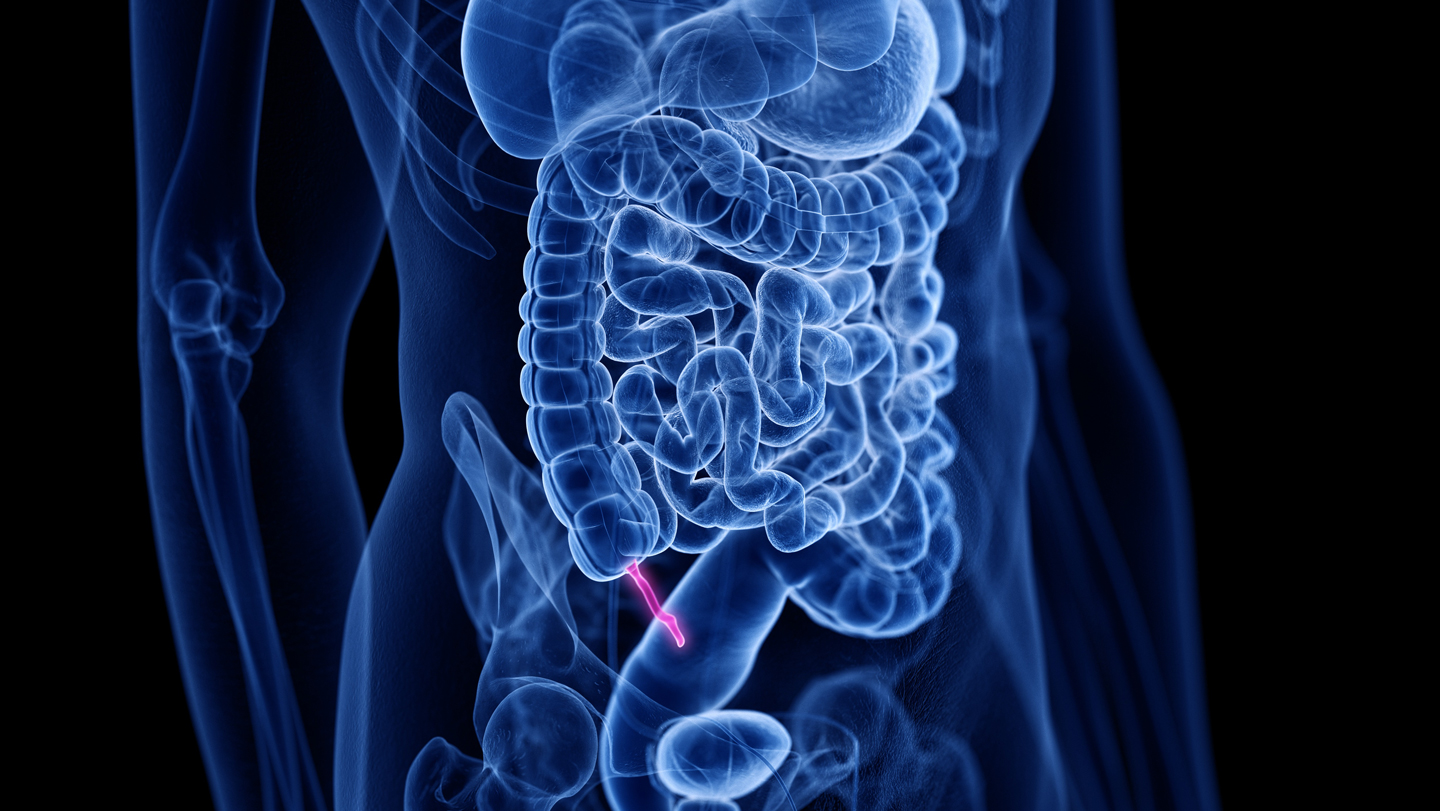
A quarter of a million people get appendicitis every year in the United States, when a blockage or infection inflames the appendix. For more than a century, doctors treating appendicitis have usually removed the organ, for fear it might rupture and cause severe infection. But in the last decade or so, trials of antibiotics have shown that appendicitis often resolves without surgery.
In 2009, researchers in Finland began the Appendicitis Acuta trial, treating 530 adults with appendicitis with either appendectomy or antibiotics. All patients were diagnosed with uncomplicated appendicitis, where the appendix is inflamed but hasn’t ruptured or developed infected pockets.
After 10 years, the team was able to contact 224 out of 257 people who’d received antibiotics, and 219 out of 273 who’d had an appendectomy. For those they couldn’t reach, they searched health records for outcomes. A total of 112 patients who’d received antibiotics ended up having an appendectomy — 70 patients in the first year, 30 people between two and five years later, and 12 people between six and 10 years later, the researchers report January 21 in JAMA.
The study protocol required an appendectomy for anyone with suspected recurrence, so it’s possible some of those additional surgeries were not needed, says principal investigator Paulina Salminen, a surgeon at the Turku University Hospital in Finland.
Two of the patients treated with antibiotics reported new complications between the five- and 10-year marks, both related to a subsequent appendectomy; two people in the appendectomy group reported new scar numbness or pain. “You don’t have to operate,” Salminen says. “The majority can be treated without appendectomy, and it is safe for the patients” in the long-term.
In addition to helping patients avoid surgery, antibiotics treatment could save money by using hospital resources more efficiently and helping people avoid sick time, Salminen says. Between 60 and 70 percent of people with acute appendicitis have the uncomplicated kind, making them eligible for antibiotics, she estimates.
The findings provide reassurance that antibiotics are a reasonable treatment, says David Flum, a surgeon at the University of Washington in Seattle. Flum is an investigator on the Comparison of Outcomes of antibiotic Drugs and Appendectomy, or CODA, trial, a U.S.-based trial modeled after the Finnish study.
The latest results are “just a little bit more reassurance for folks who want to go the antibiotic route that it’s not inevitable they’re going to have their appendix out,” he says. “That’s important.”
About 40 percent of CODA participants who’d received antibiotics had an appendectomy within one year, which increased to 49 percent by four years.
The evidence collectively shows that treatment decisions should be made in concert with the patient’s needs and priorities, he says. “There’s no one right answer here.”
Flum has developed a web-based tool to help patients learn about treatment options and to inform their decisions during discussions with their doctors. Initially, 55 percent of the 8,243 patients who accessed the site were undecided between antibiotics and surgery. Using the site reduced that indecision to 49 percent. An analysis of 356 participants who went through the decision-making process showed that more than 90 percent felt comfortable with their choice. “It didn’t freak people out,” Flum says.
Flum and Salminen are both part of a committee that announced the updated guidelines for treating appendicitis January 28 in JAMA Surgery. Previous versions have recommended antibiotics as a possible treatment. New to the guidelines is a recommendation to use shared decision making, such as the tool Flum created, in developing a treatment plan with patients.
For Salminen, even that shift is not the final step. It’s possible appendicitis can resolve with no treatment, she says. She is currently enrolling patients for a clinical trial comparing antibiotics and a placebo.
“You have to be able to think outside the box,” she says. “‘We’ve always done this’ is not a good rationale for doing something.”