People who order low-cost versions of the wildly popular weight-loss drugs Wegovy and Zepbound from so-called compounding pharmacies might soon see disruptions in their medication.
The U.S. Food and Drug Administration recently announced plans to crack down on the active pharmaceutical ingredients used in glucagonlike peptide 1 (GLP-1) drugs produced at compounding pharmacies, which make customized medications when FDA-approved drugs are unavailable. The agency’s move has unleashed a host of questions about the safety and effectiveness of compounded drugs.
What exactly does the FDA’s “notice” crack down on?
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In recent years, thousands of retailers—some legitimate and some illegal—have emerged to offer compounded versions of GLP-1 weight-loss drugs, which are typically taken in weekly injections, at extremely low prices, often without requiring a prescription. High demand for these drugs has meant that there has been “a lot of money to be made,” says Joshua King, a medical toxicologist at the University of Maryland, suggesting the financial opportunity triggered this burst of compounding pharmacies.
The FDA intends to remove questionable active ingredients from the GLP-1 drug market. But the agency’s plan could also make it more difficult for legitimate compounders to produce the drugs. The notice specifically calls out one of the biggest providers of compounded GLP-1 drugs: Hims & Hers. Just one day later, the telehealth company abruptly canceled its launch of a GLP-1 pill for weight loss. Two days later Novo Nordisk—the developer of Wegovy—filed a lawsuit accusing Hims & Hers of unlawfully mass-producing and advertising “knockoffs” of its patented drug.
“This lawsuit attacks more than just one medication or company—it directly assaults a well-established, vital component of US pharmacy practice,” wrote Hims & Hers in a statement posted on X. In an e-mail to Scientific American, Novo Nordisk’s senior vice president John F. Kuckelman wrote that “nothing in our lawsuit would prevent pharmacies from compounding other medicines to meet the needs of US patients.”
Novo Nordisk’s press release about the lawsuit mentioned the FDA’s notice. When asked by Scientific American if it was the reason for the lawsuit, the company didn’t specify.
How compounded drugs work
The FDA notice, some say, comes as the number of compounding pharmacies producing GLP-1 drugs has skyrocketed. Compounding pharmacies typically prepare versions of approved medications that are not widely available, but they can also fill in gaps in supply.
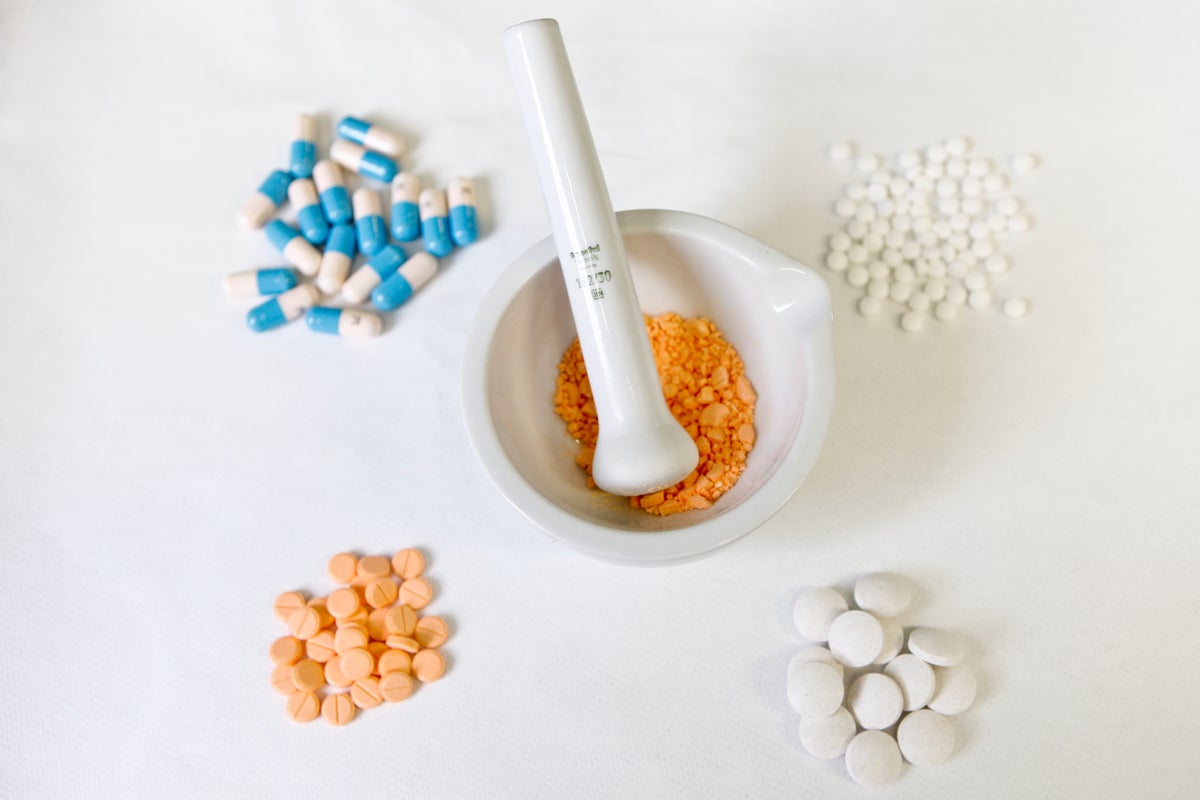
Two types exist: 503A and 503B pharmacies. A 503A compounding pharmacy makes small batches of a medication according to a doctor’s prescription to fulfill a person’s individual need—for example, a specific concentration, dosage or form of delivery (often useful for children, pets or zoo animals). If someone is unable to take a medication orally, for example, these pharmacies could create a compounded version as a cream or intravenous (IV) drip, King explains. A 503B pharmacy works on a much larger scale, using outsourcing facilities to mass-produce the compounded medications, with or without prescriptions, at a relatively low cost and to sell them to health care retailers.
The FDA does not review or approve compounded drugs, so they don’t undergo regulatory testing for safety, quality or effectiveness. The 503A compounding pharmacies are generally regulated by state pharmacy boards, whereas 503B compounders are subject to some FDA oversight. Compounded drugs shouldn’t be confused with generic drugs, which are exact copies of FDA-approved drugs whose patents have expired. Nor are they counterfeit versions of drugs.
“Not all compounding pharmacies are made the same,” says Janice Jin Hwang, a clinician and endocrinologist at the University of North Carolina at Chapel Hill. “There are some that have very good quality-control standards, but others may not.”
The scoop on compounded GLP-1 drugs
This is how the story of compounded GLP-1 drugs started: a few years ago the U.S. faced a shortage of semaglutide (the active ingredient in Wegovy and Ozempic) and tirzepatide (the active ingredient in Eli Lilly’s weight-loss drug Zepbound and its diabetes drug Mounjaro). When the FDA placed both drugs on the national shortage list in 2022, compounding pharmacies became authorized to obtain the active ingredients and produce the medications to help fill gaps in access. The FDA officially removed tirzepatide from the shortage list in December 2024 and removed semaglutide in February 2025.
Yet compounding pharmacies have continued to produce GLP-1 drugs by creating custom versions that contain certain additives and supplements. The medications might include B vitamins, marketed to alleviate nausea and gastrointestinal side effects that are associated with GLP-1 drugs, or levocarnitine, which may help with muscle wasting, says Gina Moore, a pharmacist and pharmacy law expert at the University of Colorado Anschutz. But the benefits of those additives are “theoretical,” she says. “There’s no safety or efficacy testing that go along with it.”
Are compounded GLP-1 drugs dangerous?
The safety concerns with compounded drugs aren’t hypothetical. U.S. poison centers have reported an uptick of medical issues linked to compounded GLP-1 drugs. In 2024 the FDA issued a warning about a spike in overdoses and adverse side effects that was largely attributed to dosing errors with these drugs. Unlike brand-name GLP-1 injections, which come in prefilled pens, many compounded versions come with syringes that people use to draw up medication themselves. They may also have to convert the dosage into different measurements, says King, who is medical director of the Maryland Poison Center.
“We get pictures that show instructions that say, ‘Inject 0.05 milliliters.’ A lot of patients don’t know what that means, and we’ve seen people inject 0.5 milliliters,” he says.
Experts have also raised concerns about the safety of the ingredients themselves. Many active pharmaceutical ingredients used in compounded drugs are imported from overseas facilities, which must be inspected and registered by the FDA. But with such a large volume of GLP-1 drugs moving through the system so quickly, “the FDA may not have the time or resources to inspect in as much detail,” Moore says.
The Partnership for Safe Medicines, a public health group focused on the safety of prescription drugs, conducted a review of the FDA’s freight database and found that 239 semaglutide and tirzepatide shipments—many intended for compounding—were produced at unregistered factories, facilities that the agency hasn’t inspected.
An FDA spokesperson told Scientific American that the agency monitors imported drugs and active ingredients to ensure they meet the same federal requirements as those manufactured domestically. The FDA created a “green list” alert to flag imported GLP-1 active ingredients that may have “quality concerns,” the spokesperson said, but they noted that the list does not create new limits on legal compounding of drugs.
Still, some organizations worry that the FDA’s plans to restrict the active ingredients in compounded GLP-1 drugs could affect the compounding industry at large. In a LinkedIn post, Scott Brunner, chief executive of the Alliance for Pharmacy Compounding, cautioned the FDA “not to over-correct and impede access to other compounded drugs patients need to live normal lives.”
The lowest dose of the FDA-approved Wegovy pill starts at an out-of-pocket price of $149 per month, whereas Hims & Hers had marketed its GLP-1 pill at $49 per month. Privately insured people may pay less for the brand-name drugs, says Novo Nordisk spokesperson Liz Skrbkova. “The vast majority of commercial patients pay as little as $25 a month for Wegovy. And for those [who] are not covered, they can use NovoCare,” Novo Nordisk’s direct-to-consumer pharmacy, she says. A 2025 survey by KFF reported that 27 percent of people taking GLP-1 medications who had health insurance said that they still had to pay the full cost of the drugs out of pocket, however.
Hwang is also keeping her eye on how any change to compounded GLP-1 drugs may affect access in the long run. “If I were a patient, and I had a choice of getting Wegovy versus a compounded version, of course I would get Wegovy—if the price were the same,” she says. “But the problem is making it accessible. You can’t start turning off ways of getting access to medications that are incredibly helpful for people without providing us alternative strategies.”