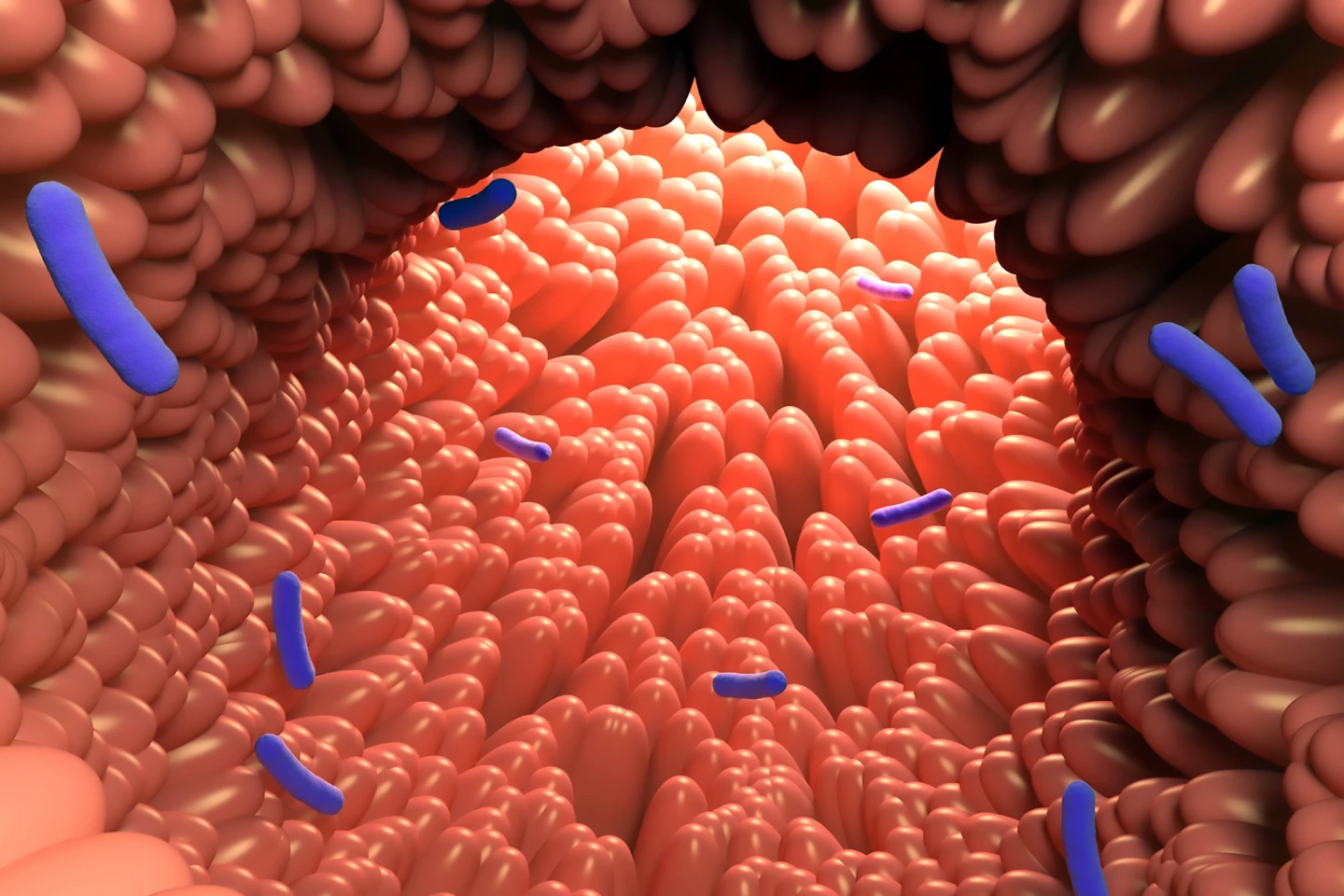
Byproducts from gut bacteria breaking down tryptophan, a dietary amino acid, can restore hormone-secreting gut cells reduced by obesity, a new study found. It opens the door to a natural, side-effect-free alternative to GLP-1 drugs like Ozempic.
Specialized gut cells called enteroendocrine cells (EECs) secrete important hormones such as glucagon-like peptide 1 (GLP-1), which help regulate insulin production and appetite. Yes, it’s the GLP-1 that drugs like Ozempic and Wegovy mimic.
New research by scientists from Marshall University, West Virginia, has uncovered how obesity significantly reduces the number of EECs, leading to metabolic dysfunction. They also found that byproducts produced by gut bacteria when they break down certain amino acids can restore them.
“Our findings suggest that microbial metabolites derived from dietary tryptophan can reverse obesity-associated reductions in hormone-secreting cells,” said Alip Borthakur, PhD, assistant professor at Marshall University’s Joan C. Edwards School of Medicine (JCESOM) and the study’s senior author. “This points to a potential therapeutic strategy that leverages gut microbes to improve metabolic outcomes in obesity.”
If you’re a fan of the TV series Seinfeld, you’d no doubt be aware of the amino acid tryptophan. In the episode “The Merv Griffin Show,” Jerry and George give a woman called Celia turkey and red wine, both containing tryptophan, to make her fall asleep so they can play with her toy collection.
What’s that stuff in turkey that makes you sleepy…
Tryptophan is an essential amino acid, meaning that the body can’t make it, and we need to get it from our diet. It plays a crucial role in making proteins and is a precursor to several important molecules, including serotonin and melatonin (presumably where the sleepy claim came from, although that has been confirmed to be a myth). Studies have shown that when gut bacteria break down tryptophan, one of the byproducts that’s produced is indole. Indole is known to regulate the gut’s immune response by activating the transcription factor aryl hydrocarbon receptor (AhR). Transcription factors are proteins that bind to DNA and regulate gene expression.
The researchers induced obesity in rats by feeding them a high-fat diet and then measured EEC levels via chromogranin A (CHGA), a marker for EECs, and levels of transcription factors that guide stem cells to become EECs. They treated human gut organoids, “mini organs” grown from healthy human colon tissue, with indole and with Lactobacillus acidophilus bacteria grown with and without tryptophan, to mimic bacterial metabolite exposure. To confirm if AhR played a role, they added an AhR antagonist called CH-223191 to block its function and measured whether it reversed the effects of indole and tryptophan metabolites.
In the obese rats, the researchers found that CHGA levels and EEC numbers dropped by around 60%. Important transcription factors for EEC differentiation were also significantly lowered. Fewer GLP-1-producing cells were found in the obese rats. In the human organoids, indole treatment significantly increased CHGA mRNA and protein, suggesting it promoted EEC formation. L. acidophilus grown with tryptophan caused a greater increase in CHGA than L. acidophilus grown without it. Blocking AhR with CH-223191 prevented these increases, confirming that AhR activation is required for the EEC-boosting effect.
There are some limitations to the study. The organoids were from healthy individuals, which limits insight into how obese tissues specifically respond to these treatments. Further, obese individuals may have altered signaling pathways that affect EEC differentiation. Also, the researchers’ focus was only on colon tissue, so results may not reflect what happens in the small intestine or other gut regions. And, although promising, results from organoids and rats may not fully translate to humans without clinical studies to confirm them.
Nonetheless, the study is important in terms of its potential real-world implications. The findings suggest a non-drug strategy for restoring GLP-1 production in obesity by encouraging the growth of tryptophan-metabolizing gut bacteria (e.g., probiotics like L. acidophilus) and using dietary supplements rich in tryptophan to fuel these bacteria. Unlike synthetic GLP-1 drugs, which can cause side effects like nausea, this approach may naturally stimulate the body’s own GLP-1 production with fewer risks. The study also highlights the potential for personalized nutrition and microbiome therapies where tailored diets or supplements are used to boost microbial production of beneficial metabolites to prevent or treat obesity and the metabolic dysfunction, such as type 2 diabetes, that often accompanies the condition.
The study was published in the International Journal of Molecular Sciences.
Source: Marshall University JCESOM
