Borrowing a cancer cell’s disguise, scientists shielded insulin-producing cells from attack by the immune system, a breakthrough that could pave the way for targeted type 1 diabetes treatments without whole-body immunosuppression.
There has been a lot of research into understanding how cancer evades the body’s immune system, and the ways that science might be able to get around that. One of the ways cancer hides itself in the body is by attaching sugar molecules to the surface of its cells.
Now, a group of researchers from the Mayo Clinic has applied that knowledge, and the sneaky immune-system-avoiding trick used by cancer, to develop a treatment for type 1 diabetes.
“Our findings show that it’s possible to engineer beta cells that do not prompt an immune response,” said Virginia Shapiro, PhD, an immunology researcher and the study’s corresponding author.
ST8Sia6 is an enzyme, a type of protein, whose job is to attach special sugar molecules called sialic acids to the surface of cells. It works inside the cells’ “packaging” area, the Golgi apparatus, before proteins reach the cell surface. By adding sialic acids, ST8Sia6 changes how cells look to the immune system. These sugars act like tags or shields that send a “don’t attack me!” signal to certain immune cells. The immune cells that read this shield use special receptors called sialic acid-binding immunoglobulin-type lectins, Siglecs that, when they bind to these sugars, usually tell the immune system to calm down and not launch an attack.
In healthy tissues, this process helps prevent unnecessary immune damage. However, some cancers produce more ST8Sia6 than normal, which increases the “don’t attack me!” signals on the cancer cell surface. Immune cells, such as T cells, bind to these extra sugars through the Siglec receptors, which sends an “off” signal. As a result, the immune system ignores or tolerates the cancer cells instead of killing them.
Mayo Clinic
“The expression of this enzyme basically ‘sugar coats’ cancer cells and can help protect an abnormal cell from a normal immune response,” Shapiro said. “We wondered if the same enzyme might also protect a normal cell from an abnormal immune response.”
In type 1 diabetes (T1D), the immune system mistakenly thinks the insulin-producing beta cells in the pancreas are dangerous, so it sends immune cells to attack and destroy them. Once the beta cells are gone, the body can’t make insulin, and blood sugar control is lost.
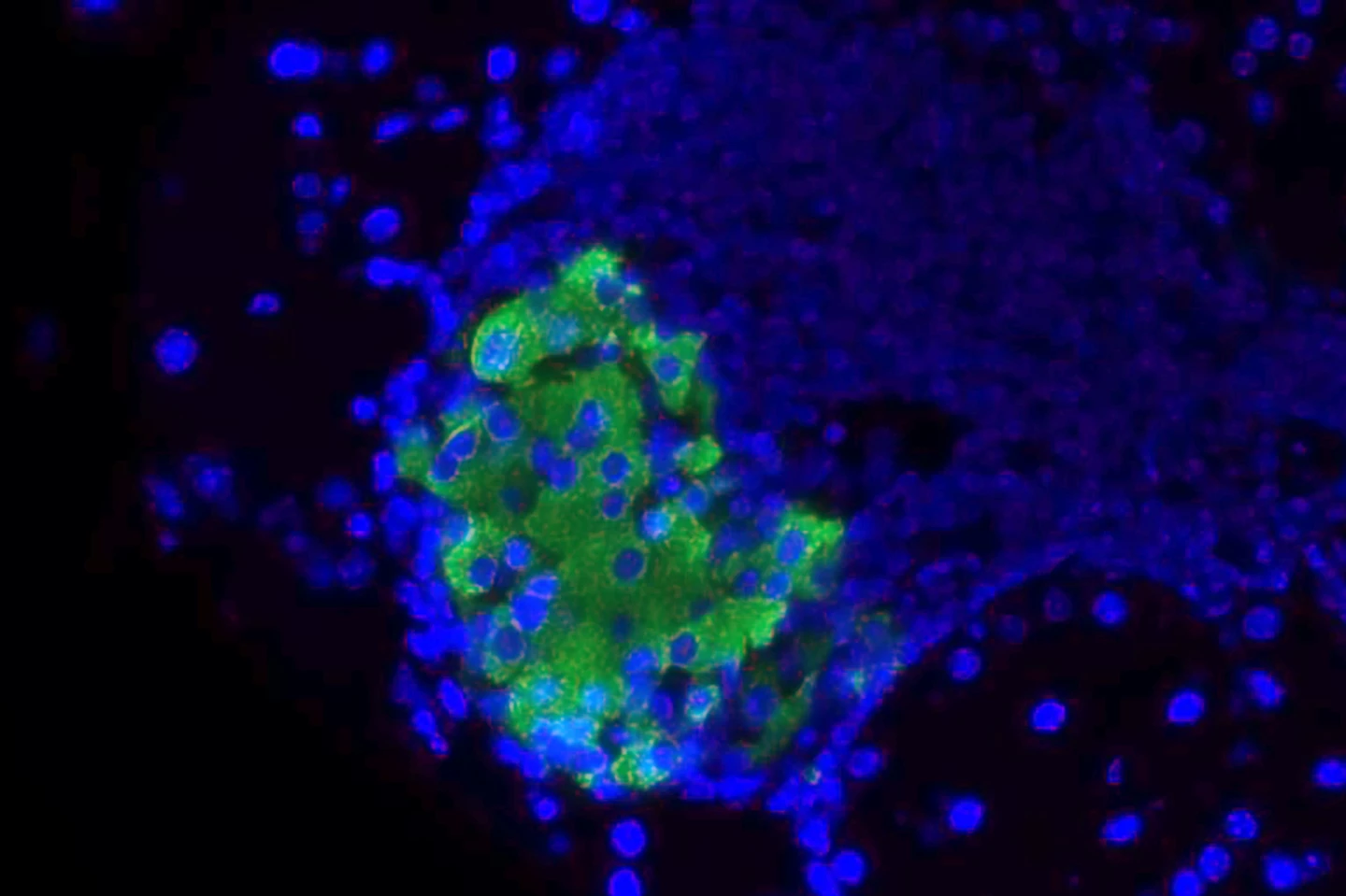
The researchers used non-obese diabetic (NOD) mice, a well-established model for human T1D, and genetically modified them to express ST8Sia6 specifically in pancreatic beta cells. The expression could be turned on or off using the antibiotic doxycycline, which allowed for time-specific testing. They monitored diabetes onset via blood glucose levels, microscopically analyzed the animals’ beta cells, profiled the immune cells, and measured inflammation and antibody levels.
Only 6% of genetically modified female NOD mice developed diabetes, compared to 60% of control mice – a 90% reduction in disease incidence. Male mice were also protected, though less dramatically, likely due to natural sex differences in the mouse models. The researchers observed that in genetically modified mice, beta cells were preserved into old age (300 days), while in control mice, they were largely destroyed.
Despite having normal levels of autoantibodies and autoreactive T cells – indicative of an autoimmune response – the genetically modified mice didn’t experience progressive insulitis, which is when the immune cells infiltrate the pancreas islets, clusters of cells in which beta cells are located. Immune protection conferred by ST8Sia6 was restricted to the islets; other organs still showed signs of autoimmunity.
“Though the beta cells were spared, the immune system remained intact,” said lead author Justin Choe, a Mayo Clinic MD-PhD program student, studying at the Graduate School of Biomedical Sciences and the Alix School of Medicine. “We found that the enzyme specifically generated tolerance against autoimmune rejection of the beta cell, providing local and quite specific protection against type 1 diabetes.”

The immune protection seen by the researchers came from modifying the local immune environment, not from removing autoreactive immune cells entirely. The enzyme specifically reduced pro-inflammatory cells and the production of IL-12p35, a cytokine or chemical messenger that’s crucial for promoting inflammation. Additionally, it altered the balance in the islets towards regulatory T cells (Tregs), which suppress inflammation. Switching off ST8Sia6 expression at 20 weeks still preserved the protection, suggesting that early intervention was sufficient to induce long-lasting immune tolerance.
There are some limitations to the study. Primarily, the NOD mouse model doesn’t perfectly replicate human T1D, especially due to differences like the female-biased disease progression that isn’t seen in humans. And effects seen in mouse immune systems may not directly apply to humans. Also, while the immune protection was strong in the pancreatic islets, other autoimmune manifestations continued, which highlights the specificity of the protection but also potential gaps. And, the study didn’t fully evaluate long-term immune suppression risks, although no major systemic suppression was observed.
Putting aside these limitations, though, this research offers a potential breakthrough in treating or even preventing T1D via localized immune system modulation. It could also boost the success of pancreatic islet cell transplantation by protecting transplanted cells from immune attack without suppressing the immune system across the entire body.
“A goal would be to provide transplantable cells without the need for immunosuppression,” said Shapiro. “Though we’re still in the early stages, this study may be one step toward improving care.”
The study was published in The Journal of Clinical Investigation.
Source: Mayo Clinic